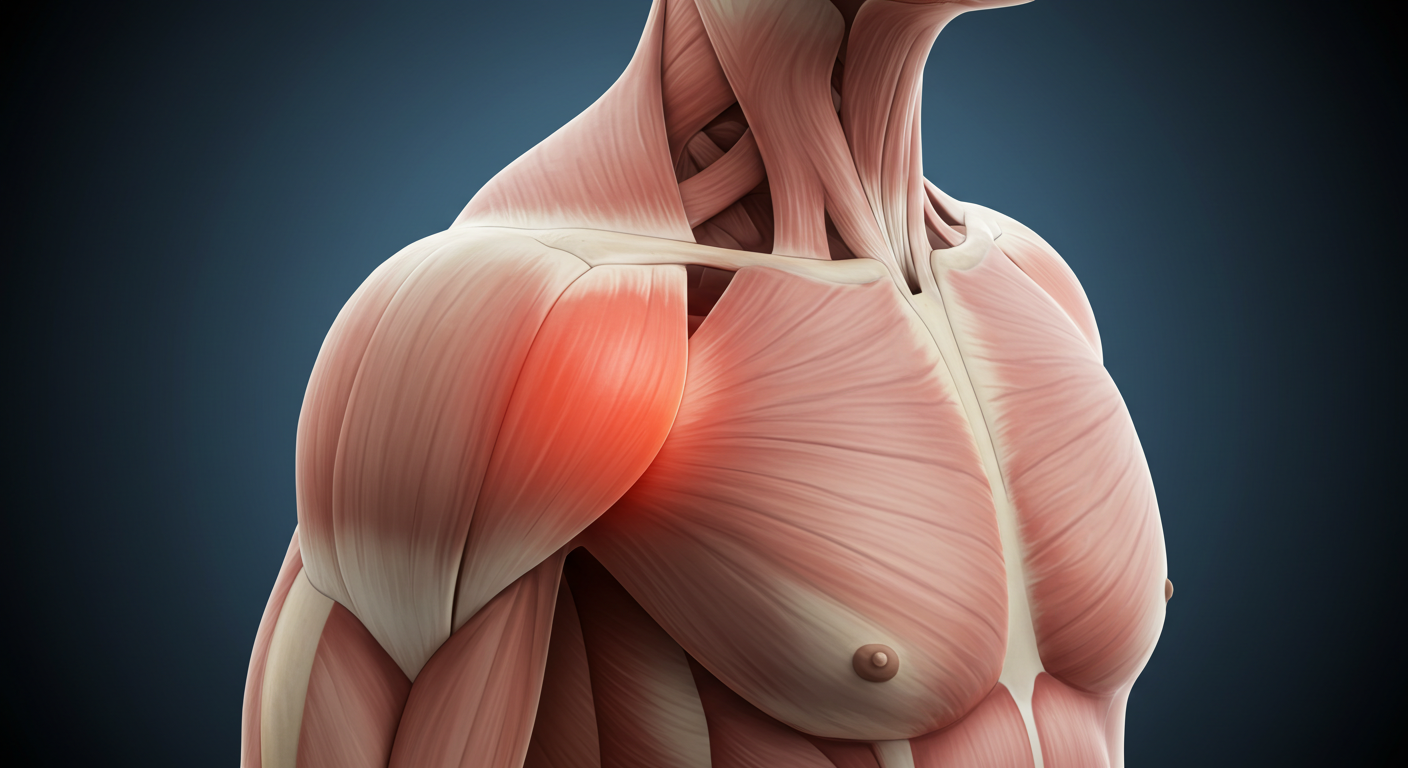
Shoulder Trigger Points
Shoulder trigger points are tight, hyperirritable spots in muscle fibers—often forming in the upper trapezius, deltoid, and rotator cuff muscles. These “knots” can cause stiffness, tension, weakness, and referred pain down the arm, even when your joint is healthy.
OVERVIEW
SYMPTOMS
Shoulder trigger point symptoms can range from mild discomfort to intense, radiating pain. These muscle knots often cause referred pain, meaning the discomfort may not stay in the shoulder but travel down the arm or up into the neck. Identifying common shoulder pain symptoms caused by trigger points is key to getting the right treatment.
-
Localized tight knots that may feel tender or hard under the skin
-
Referred pain: ache, tingling, or numbness radiating from the shoulder down the arm
-
Shoulder stiffness, limited range of motion, or weakness
-
Headaches originating from shoulder/neck tension
-
Two types:
-
Active trigger points: painful even without pressure, often sending pain into the arm
-
Latent trigger points: only painful when pressed
-
CAUSES
The most common causes of shoulder trigger points include overuse, poor posture, and muscle imbalances. These factors place stress on shoulder muscles like the upper trapezius and rotator cuff, eventually leading to painful knots. Understanding what contributes to shoulder muscle tension can help you prevent future issues.
- Overuse or repetitive motions (e.g. heavy lifting, keyboard use)
-
Poor posture, especially forward head and rounded shoulders
-
Stress-induced muscle tension
-
Muscle imbalances, such as weak shoulder stabilizers or tight chest muscles
-
Injury or trauma, including micro-tears or strains
DIAGNOSIS
Proper diagnosis of shoulder trigger points involves a hands-on assessment of muscle tightness, pain referral patterns, and range of motion. Since trigger point pain can mimic other shoulder or nerve conditions, it’s important to rule out joint problems or injuries to ensure accurate treatment.
-
Physical examination: finding tender muscle knots and observing referred pain patterns
-
Functional tests: assessing weakness or motion limitations
-
Exclusion of joint issues through palpation and, when needed, imaging (e.g. X‑ray, MRI)
FAQs
Q: Can trigger points cause arm or hand symptoms?
Yes—especially active trigger points, which can refer pain, tingling, or numbness down the arm .
Q: How long do trigger points last?
They can linger for weeks to months—but combining manual therapies, targeted exercises, and posture correction often speeds recovery.
Q: Are trigger points permanent?
No—treatment and good habits (ergonomics, strength, stress management) can resolve them and reduce recurrence.
Q: Can I self-treat shoulder trigger points?
Yes—gentle self-massage with tools like a tennis ball, stretching, and applying heat can help. But professional treatment ensures a complete approach.

EVALUATION
When evaluating shoulder trigger points, practitioners typically:
-
Identify active vs. latent trigger points
-
Map where pain refers
-
Measure range of motion and strength
-
Review patient history for repetitive use, posture habits, or stress factors

CMT + THERAPIES
-
Chiropractic Manipulative Therapy (CMT): Adjustments to cervical or thoracic spine to restore alignment and reduce muscle stress
-
Trigger-point massage: Deep pressure or sustained compression to release knots
-
Myofascial release and soft-tissue mobilization
-
Dry needling: Fine needles inserted into trigger points to release muscle tension
-
Therapeutic ultrasound: Helps improve blood flow to tight areas
-
Stretching and strengthening exercises: Focus on scapular stabilizers, rotator cuff, and posterior shoulder
-
Posture correction: Ergonomic coaching; strengthening upper back and neck muscles

PREVENTION + ERGONOMICS TIPS
-
Maintain good posture: sit upright, shoulders back, head aligned over spine
-
Create an ergonomic workspace: monitor at eye level, forearms parallel to floor, chair supporting lower back
-
Take frequent breaks (every 30–60 minutes) to stretch or walk
-
Incorporate daily shoulder and neck stretches—especially after prolonged sitting
-
Strengthen scapular muscles, rotator cuff, and core
-
Practice relaxation techniques to reduce stress-related muscle tension
-
Use proper lifting techniques: lift with legs, keep shoulders down/back
OUR ELITE APPROACH

STEP ONE:
PAIN RELIEF
Fix your pain without pills or surgery and get you back to life, sport, or work. We’re trying to get your pain under control and start you on your way to a full recovery.

STEP TWO:
RETURN TO FUNCTION

